Trump administration cools on Mississippi Medicaid work requirements
Published 10:36 am Friday, May 11, 2018
By Mississippi Today
WASHINGTON, D.C. — For months, Mississippi’s application for a program that would require certain Medicaid recipients to work has been considered a lock by supporters and opponents of the program.
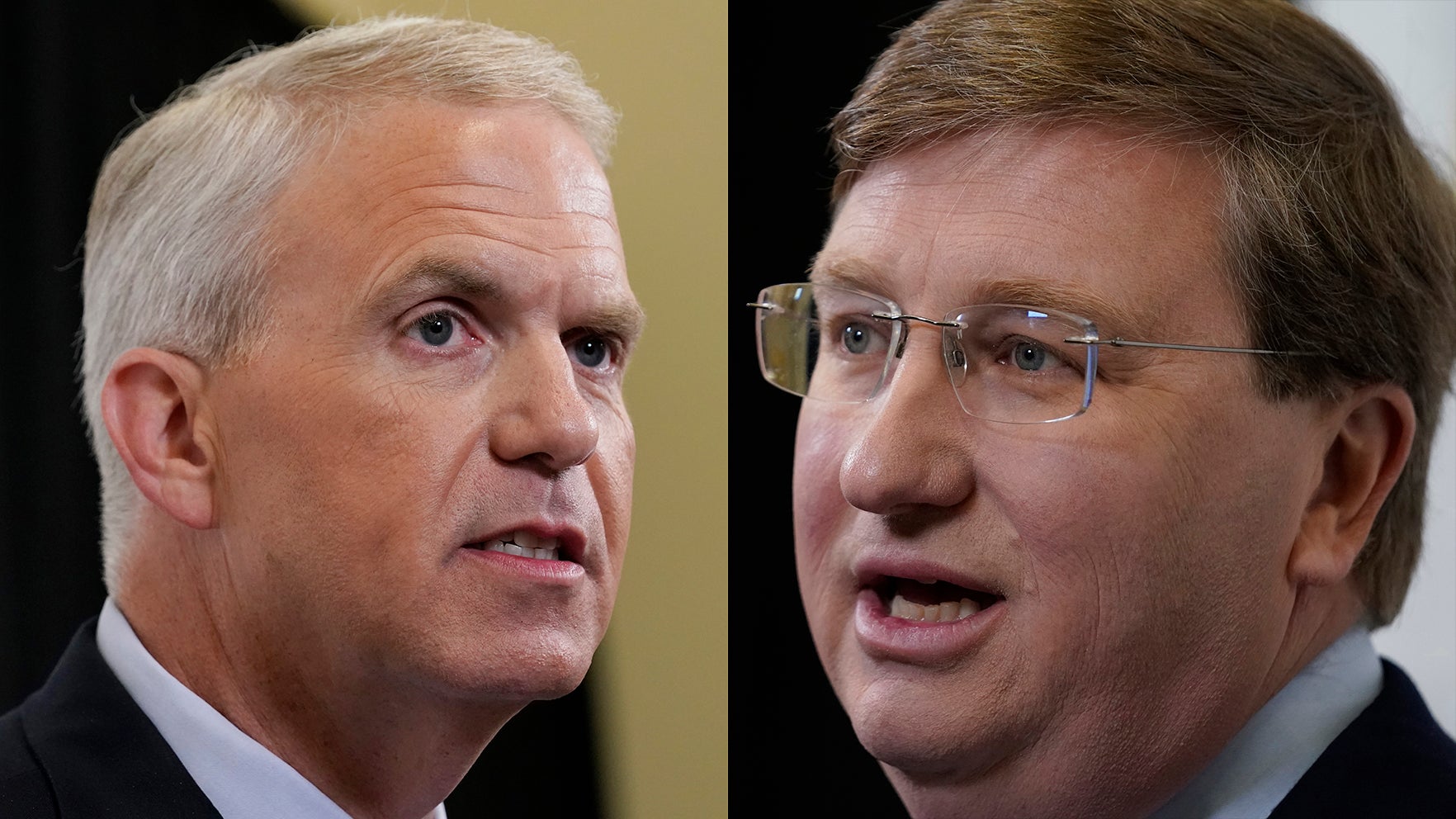
But last week the Trump Administration walked back support for the waivers in states like Mississippi that have opted out of Medicaid expansion, placing a question mark over a controversial program that has the strong support of Gov. Phil Bryant.
Last week Seema Verma, administrator for the federal Centers for Medicare and Medicaid Services, warned non-expansion states that their waiver applications would need to include a plan to avoid the “subsidy cliff,” in which a person earns too much to keep their Medicaid coverage and too little to qualify for a tax credit on the insurance exchange. Like many conservatives, Verma had long endorsed Medicaid work requirements, saying they “promote community engagement.” But last week’s comments echoed critics of the waiver program who have argued that work requirements could force more than 20,000 Mississippians out of the Medicaid program.
Mississippi’s application, which was submitted in November and is still waiting on CMS approval, does not currently contain a plan to address a “subsidy cliff.” But the Division of Medicaid told Mississippi Today in a statement that it was currently working with CMS to meet this standard:
“The Mississippi Division of Medicaid is working with the Trump Administration to ensure that the Mississippi Medicaid Workforce Training Initiative offers a responsible path to greater self-sufficiency and well-being. We are not opposed to making adjustments to the waiver application to achieve this goal and are actively working to refine the application where possible.”
The governor’s office did not respond to requests for comment.
Although Verma’s comments last week were the first time that an official from the Trump Administration has publicly acknowledged that these work requirements could leave some beneficiaries uninsured, concern about a subsidy cliff in non-expansion states is not new within the health care community.
Currently, only four states, Kentucky, Arkansas, Indiana and New Hampshire, have had their waiver requests approved. All are states that expanded Medicaid. Approval of Mississippi’s application, which is one of three from non-expansion states, is pending.
In those expansion states, anyone can qualify for Medicaid if their earned income is too low to receive a subsidy on the state insurance exchange. But in Mississippi, a non-expansion state, the only adults who qualify for Medicaid are either pregnant women, elderly or disabled. The one exception is low-income parents or caretakers, who account for just seven percent of the 700,000 Medicaid beneficiaries in the state.
This is the population targeted by the work requirements, which would require these recipients to work or volunteer 20 hours a week or to participate in job training in order to keep coverage. The catch is that income limits for these individuals are so low — as little as $306 a month — that even a minimum wage job would make a beneficiary ineligible for Medicaid. This is Verma’s “subsidy cliff,” where a person would earn too much to qualify for Medicaid and too little to qualify for a tax credit.
In Mississippi, approximately 50,000 people fall into this category, and an April report from Georgetown University’s Center for Children and Families estimated that, if the federal government approves Mississippi’s application as written, as many as half of them could lose their coverage over the next five years.
“They claim the waiver will help people build a foundation for health, and that imposing a work requirement makes it somehow possible to have coverage. But in reality it makes it impossible for that population to have both employment and Medicaid coverage,” said Roy Mitchell, executive director of the Mississippi Health Advocacy Program.
“If these programs are implemented as written, I predict you’re going to see legislators running for the exits.”
CMS did not respond to a request to clarify how the Division of Medicaid would need to change its application. Currently, Medicaid offers transitional insurance, covering an individual for the first 12 months after they leave the program. But Mitchell said it was unlikely that someone would go from unemployed to a job that offers health insurance benefits in just one year.
“It’s going to take a lot to implement this (and) in a state that has very few jobs to provide health insurance, I might add,” Mitchell said.
Still, Mississippi’s application for a waiver, in its current form, was considered all but guaranteed by the program’s biggest supporters and critics. In his January State of the State speech, Bryant dismissed the controversy, arguing that work requirements are not intended as a “punitive action” but instead to “help this population reap the rewards of a good job, and one day receive health care coverage from their employer, not the state or federal government.”
Last month, Georgetown University released a detailed report on the effects of these work requirements to Medicaid beneficiaries. Joan Alker, executive director for the Center for Children and Families at Georgetown, acknowledged that approval wasn’t guaranteed for work requirement waivers in states that didn’t expand Medicaid. But she said that Mississippi’s application was closer to approval than any other application from a non-expansion state.
“Mississippi’s proposal has been through the state and federal public comment process. Mississippi is ahead of Alabama in the queue and the key one to watch,” Alker said.
Despite concern over the consequences of requiring recipients of Mississippi Medicaid to work to keep their insurance, the Trump Administration has never explicitly said it intended its waiver program for non-expansion states.
In fact, when Verma announced the program in November, she described it as a response to Medicaid expansion, which had “moved millions of working-age, non-disabled adults into a program that was created to care for seniors in need, pregnant mothers, children and people with disabilities.”
A brief submitted by the Trump Administration late last month expanded on this idea. In the lawsuit, Stewart v. Azar, a group of Kentucky Medicaid recipients are suing the federal government over their state’s recently approved work requirement. But in their defense of the waiver, attorneys for the federal Department of Health and Human Services defined the program as “an experimental project” that would encourage “members of the Medicaid expansion population to engage in healthy behaviors.”
Jameson Taylor, vice president of the Mississippi Center for Public Policy, a conservative think tank, has long supported implementing a Medicaid work requirement in Mississippi. But he acknowledged Wednesday that the Trump Administration may be currently concentrating their energy on states that had opted to expand their Medicaid programs.
“But just because the White House is saying we’re more comfortable with work requirements in expansion states than non-expansion states doesn’t mean we’re never going to have a work requirement here. It just means it may take more time,” Taylor said.